Now that you've reached the third trimester, you're in the home stretch of your pregnancy. You've only got a few more weeks to go, but this part of your pregnancy can be the most challenging.
In this article, you'll learn what to expect during your third trimester of pregnancy. You'll find out which symptoms are normal, and which ones may warrant a call to your doctor.
Changes in Your Body
Backache. The extra weight you've gained is putting added pressure on your back, making it feel achy and sore. You might also feel discomfort in your pelvis and hips as your ligaments loosen to prepare for labor. To ease the pressure on your back, practice good posture. Sit up straight and use a chair that provides good back support. At night,sleep on your side with a pillow tucked between your legs. Wear low-heeled, comfortable shoes with good arch support. To relieveback pain, use a heating pad and ask your doctor whether it's OK for you to take acetaminophen.
Bleeding. Spotting may sometimes be a sign of a serious problem, including placenta previa (the placenta grows low and covers the cervix ), placental abruption (separation of the placenta from the uterine wall), or preterm labor . Call your doctor as soon as you notice any bleeding.
Braxton Hicks contractions. You might start to feel mild contractions, which are warm-ups to prepare your uterus for the real labor to come. Braxton Hicks contractions often aren't as intense as real labor contractions, but they may feel a lot like labor and can eventually progress to it. One main difference is that real contractions gradually get closer and closer together -- and more intense. If you're red in the face and out of breath after your contractions, or they're coming regularly, call your doctor.
Breast enlargement. By the end of your pregnancy, your breasts will have grown by as much as 2 pounds. Make sure you're wearing a supportive bra so your back doesn't suffer. Close to your due date , you may start to see a yellowish fluid leaking from your nipples. This substance, called colostrum, will nourish your baby in the first few days after birth.
Discharge . You might see more vaginal discharge during the third trimester. If the flow is heavy enough to soak through your panty liners, call your doctor. Close to your delivery date, you might see a thick, clear, or slightly blood-tinged discharge. This is your mucus plug, and it's a sign that your cervix has begun dilating in preparation for labor. If you experience a sudden rush of fluid, it may mean that your water has broken (although only about 8% of pregnant women have their water break before contractions begin). Call your doctor as soon as possible after your water breaks.
Fatigue. You might have been feeling energetic in your second trimester, but are weary now. Carrying extra weight, waking up several times during the night to go to the bathroom, and dealing with the anxiety of preparing for a baby can all take a toll on your energy level. Eat healthy food and get regular exercise to give yourself a boost. When you feel tired, try to take a nap, or at least sit down and relax for a few minutes. You need to reserve all your strength now for when your baby arrives and you're really not getting any sleep.
Frequent urination . Now that your baby is bigger, the baby's head may be pressing down on your bladder . That extra pressure means you'll have to go to the bathroom more frequently -- including several times each night. You might also find that you're leaking urine when you cough , sneeze, laugh, or exercise. To relieve the pressure and prevent leakage, go to the bathroom whenever you feel the urge and urinate completely each time. Avoid drinking fluids right before bedtime to cut down on unwanted late-night bathroom visits. Wear a panty liner to absorb any leakage that does occur. Let your doctor know if you experience any pain or burning with urination. These can be signs of a urinary tract infection.
Heartburn and constipation . They're caused by extra production of the hormone progesterone, which relaxes certain muscles -- including the muscles in your esophagus that normally keep food and acids down in your stomach , and the ones that move digested food through your intestines . To relieve heartburn, try eating more frequent, smaller meals throughout the day and avoid greasy, spicy, and acidic foods (like citrus fruits). For constipation, increase your fiber intake and drink extra fluids to keep things moving more smoothly. If your heartburn or constipation is really bothering you, talk to your doctor about what medications may be safe for you to take for symptom relief.
Hemorrhoids . Hemorrhoids are actually varicose veins -- swollen veins that form around the anus. These veins enlarge during pregnancy because extra blood is flowing through them and the weight of pregnancy increases the amount of pressure to the area. To relieve the itch and discomfort, try sitting in a warm tub or sitz bath. Ask your doctor whether you can also try an over-the-counter hemorrhoid ointment or stool softener.
Shortness of breath. As your uterus expands, it rises up until it sits just under your rib cage, leaving less room for your lungs to expand. That added pressure on your lungs can make it more difficult to breathe. Exercising can help with shortness of breath. You can also try propping up your head and shoulders with pillows while you sleep.
Spider and varicose veins. Your circulation has increased to send extra blood to your growing baby. That excess blood flow can cause tiny red veins, known as spider veins, to appear on your skin . Spider veins may get worse in your third trimester, but they should fade once your baby is born. Pressure on your legs from your growing baby may also cause some surface veins in your legs to become swollen and blue or purple. These are called varicose veins. Although there's no way to avoid varicose veins, you can prevent them from getting worse by:
- Getting up and moving throughout the day
- Wearing support hose
- Propping up your legs whenever you have to sit for long periods of time.
Varicose veins should improve within a few months after you deliver.
Swelling. Your rings might be feeling tighter these days, and you may also notice that your ankles and face are looking bloated. Mild swelling is the result of excess fluid retention ( edema ). To reduce swelling, put your feet up on a stool or box whenever you sit for any length of time, and elevate your feet while you sleep. If you have sudden onset of swelling though, seek medical attention immediately as it may be a sign of preeclampsia, a dangerous pregnancy complication.
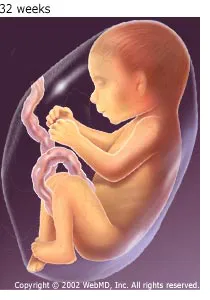
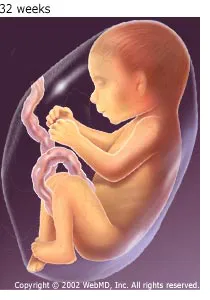
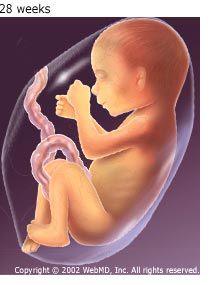
Weight gain. Aim for a weight gain of 1/2 pound to 1 pound a week during your third trimester. By the end of your pregnancy, you should have put on a total of about 25 to 35 pounds (your doctor may have recommended that you gain more or less weight if you started out your pregnancy underweight or overweight ). The extra pounds you've put on are made up of the baby's weight, plus the placenta, amniotic fluid , increased blood and fluid volume, and added breast tissue. If your baby seems to be too small or too big based on the size of your belly, your doctor will do an ultrasound to check his growth.
Red Flag Symptoms
Any of these symptoms could be a sign that something is wrong with your pregnancy. Don't wait for your regular prenatal visit to talk about it. Call your doctor right away if you experience:
- Severe abdominal pain or cramps
- Severe nausea or vomiting
- Bleeding
- Severe dizziness
- Pain or burning during urination
- Rapid weight gain (more than 6.5 pounds per month) or too little weight gain